In one example, primary care physicians can earn up to $252,379 more annually by working in the highest-paying state in the PCP category (Mississippi) than in the lowest-paying state (Alaska)
by Intelliworx
The delta between the highest and lowest compensation among providers is staggering. You might think a provider stands to make more income working for a big city hospital than they do in a rural community, but that’s not always the case.
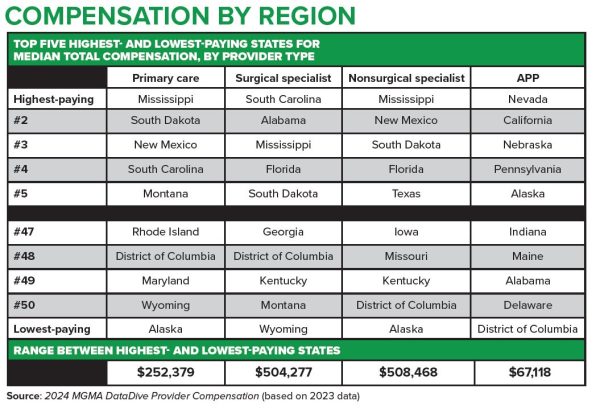
Consider the following data – derived from the 2024 MGMA provider compensation data:
- Primary care physicians (PCP) can earn up to $252,379 more annually by working in the highest-paying state in the PCP category (Mississippi) than in the lowest-paying state (Alaska);
- Surgical specialists can earn up to $504,277 more annually by working in the highest-paying state in the surgical category (South Carolina) than in the lowest-paying state (Wyoming);
- Non-surgical specialists can earn up to $508,468 more annually by working in the highest-paying state in the non-surgical category (Mississippi) than in the lowest-paying state (Alaska); and
- Advanced practice providers (APPs), such as nurse practitioners (NPs) and physician assistants (PAs) can earn up to $67,118 more annually by working in the highest-paying state in the APP category (Nevada) than in the lowest-paying territory (Washington, DC).
Here’s what that looks like graphically:
(Click for Larger Image)
While many healthcare providers choose to work in medicine for altruistic reasons, provider compensation is still important. Other studies show compensation is frequently the top reason why a provider takes a job, stays in that job or chooses to leave for another.
They earn it too – provider productivity has skyrocketed in recent years. This is a group of people that literally make life-and-death decisions frequently. Moreover, it takes years of schooling to become a provider, and many graduates carry large student loan balances that need to be repaid. And there’s burnout too. Especially given the pressure to see more patients in the same amount of time.
(It’s worth noting the Department of Veteran’s Affairs offers many healthcare scholarships to support their needs in caring for our nation’s veterans; coincidentally, the VA uses one of our software solutions to manage their scholarship program).
Rural healthcare facilities tend to have a lower volume of patients, which means they make less revenue and sometimes struggle to match compensation benchmarks. However, it’s worth pointing out that the lower cost of living in a rural area can often make a difference in what’s left of a paycheck after paying the bills.
Indeed, other surveys exploring the top recruiting challenges for rural healthcare suggest that the lower cost of living, greater autonomy, and a higher sense of fulfillment are attractive characteristics rural healthcare facilities should pitch to prospective provider candidates.
As for the MGMA compensation data, a copy of the full report, titled “Provider Pay and the Dawn of a New Era of Productivity,” is freely available for download with registration on the MGMA website.
* * *
Our Healthcare Workforce Management software solution is designed to facilitate provider recruiting for rural healthcare facilities. Contact us for a no-obligation demo.
If you enjoyed this post, you might also like:
With all eyes on recruiting, healthcare also has a retention problem
Image credits: Pexels and cited report by MGMA