New survey finds one in four healthcare organizations experience as much as $1 million (or more) annually in lost billings due to credentialing
Healthcare organizations report completing provider credentialing faster than in prior years and expressed confidence in their processes. Even so, more than one-third of respondents experience lost billings as a result of credentialing challenges.
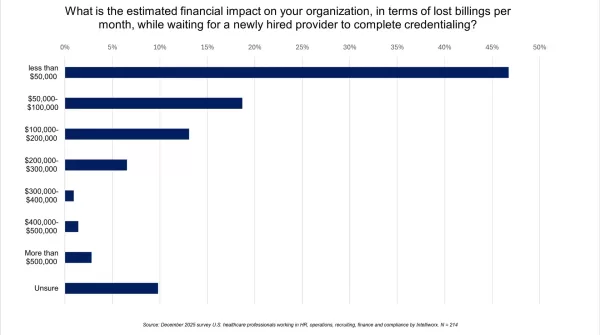
That’s according to a new survey we commissioned of human resources, operations and finance professionals working for U.S. healthcare organizations. More than four in 10 (43%) of respondents said their organization experiences $50,000 or more in lost billings every month as a result of credentialing issues. Further, one in four (25%), experience lost billings to the tune of $100,000 a month or more.
When considering the impact on a yearly basis, those losses in monthly billing quickly add up to seven figures. The contrast between the confidence expressed in the process and the financial impact suggests there’s a ‘credentialing paradox’ which, if addressed, could help improve margins for healthcare organizations.
Below is a breakdown of what the survey found.
Stay in touch by subscribing to our email newsletter.
We will never share or sell your email address.
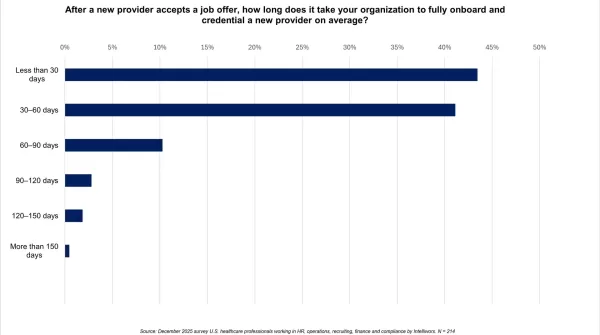
1/ How long does it take to credential a new provider?
Respondents indicated they are credentialing providers at a faster pace than in prior years. A plurality of respondents (43%) said credentialing a new provider takes just 30 days or less. Another 41% said the process takes 30-60 days. About 15% said the process takes 60 days or more, which is more in line with traditional benchmarks.
Q1: After a new provider accepts a job offer, how long does it take your organization to fully onboard and credential a new provider on average?
-
- 43% said credentialing a new provider takes less than 30 days;
- 41% said credentialing a new provider takes 30–60 days;
- 10% said credentialing a new provider takes 60–90 days;
- 3% said credentialing a new provider takes 90–120 days;
- 2% said credentialing a new provider takes 120–150 days; and
- 0.5% said credentialing a new provider takes more than 150 days.
These are surprising findings relative to other benchmarking surveys. We’ve previously summarized three other outside healthcare surveys that suggest credentialing, historically, has required much more time.
For example, MGMA surveyed 425 medical practices in 2021 and found payers take as long as 100 days to credential providers.
Similarly, a 2023 survey “of more than 2,000 internal physicians and provider recruitment professionals” by AAPPR found credentialing takes 1-3 months on average. Another 24%, in that survey, said the process lasts 4-6 months.
Finally, a 2024 AAPPR poll of “167 recruitment professionals” revealed that 70% of responding healthcare organizations say this process takes three to four months.
While surveys themselves can account for some differences in the findings – i.e., who is answering the questions and how the question was asked – completing credentialing in under 30 days sounds very optimistic.
(Click for larger image)
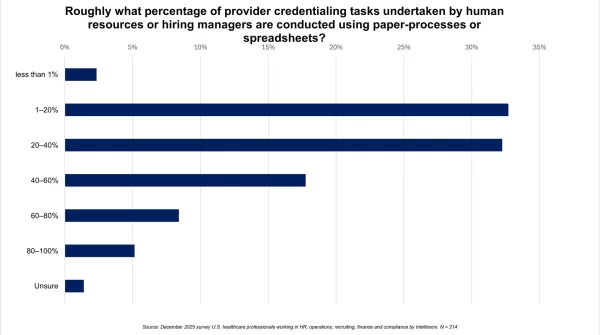
2/ What percentage of credentialing tasks are completed manually?
A significant piece of the credentialing process is handled manually, including passing paper around or using spreadsheets. Our survey found 64% of respondents say 20% or more of credentialing tasks are done manually. About one-third (31%) put that number at more than 40%. Finally, another 13% say their credentialing process is more than 60% manual.
Q2: Roughly what percentage of provider credentialing tasks undertaken by human resources or hiring managers are conducted using paper-processes or spreadsheets? (choose one)
-
- 2% said less than 1% of their credentialing process is manual;
- 33% said between 1–20% of their credentialing process is manual;
- 32% said between 20–40% of their credentialing process is manual;
- 18% said between 40–60% of their credentialing process is manual;
- 8% said between 60–80% of their credentialing process is manual;
- 5% said between 80–100% of their credentialing process is manual; and
- 1% were unsure of the answer to this question.
Based on open-ended comments, respondents were clearly interested in automation to assist with this process. Among the verbatim comments were the following:
- “Automation with notifications of [credentialing] expiration.”
- “Communication [integration] between job boards and ATS [applicant tracking system].”
- “More automated process.”
- “I’d like for things to go through faster; AI is helping a lot. I hope that we get a good balance of AI with human oversight.”
- “More streamlined and quicker process.”
- “[Better] candidate communication and engagement.”
- “I want to buy a subscription service to a place that could do it all at once, that’d be very nice and convenient.”
(Click for larger image)
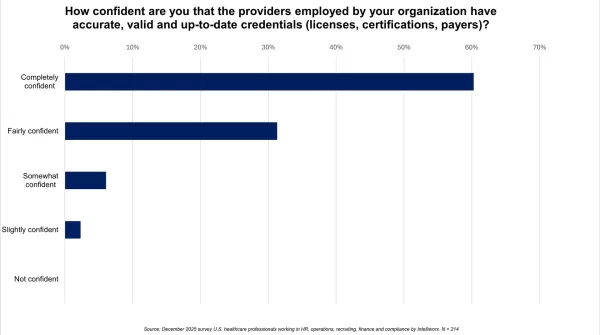
3/ How confident are you that your providers’ credentials are current?
A majority of respondents (60%) are “completely confident” that providers have their credentials up to date. Another 31% are “fairly confident” that all provider credentials are current. This seems reasonable given the importance of credentials to a healthcare facility’s ability to generate revenue.
Q3: How confident are you that the providers employed by your organization have accurate, valid and up-to-date credentials (licenses, certifications, payers)? (choose one)
-
- 60% said they were “completely confident” credentials were current;
- 31% said they were “fairly confident” credentials were current;
- 6% said they were “somewhat confident” credentials were current; and
- 2% said they were “slightly confident” credentials were current.
No respondent indicated they were “not confident” or “unsure.” This turned out to be a hinge in the findings, as we’ll get into next.
(Click for larger image)
4/ Have credentialing errors resulted in reimbursement delays?
More than one-third of respondents (34%) experience financial issues as a result of credentialing challenges. On the flip side, some 64% said they “rarely” or “never” have issues.
Even so, a comparison between the answers to this question – with answers to prior questions – suggests some organizations might be over-confident in their credentialing process. Given how closely tied credentials are to revenue and the substantial reliance on manual processes, there is clearly room for improvement.
Q4: Have you ever experienced a payer reimbursement delay, audit issue, or penalty due to onboarding, credentialing or enrollment errors?
-
- 3% said they “always” have reimbursement delays;
- 8% said they “often” have reimbursement delays;
- 22% said they “sometimes” have reimbursement delays;
- 39% said they “rarely” have reimbursement delays;
- 26% said they “never” have reimbursement delays; and
- 2% said they were “unsure” if they have reimbursement delays.
In open-ended remarks, some respondents suggested that payers were responsible for slow-walking credentials in order to delay reimbursement. One called for a “time limit” to be imposed that would require payers to respond to credentialing requests on a deadline.
Other respondents indicated a desire to see credentials before making a job offer (this exists today). A few respondents suggested providers could help expedite the process by having their paperwork together and ready to be submitted at the time of hire.
A third theme pointed to the process itself. For example, one respondent noted that credentialing packets in general require more paperwork, and varying degrees of paperwork, than is truly necessary. Another called for a single standard federal system to complete credentialing nationwide.
(Click for larger image)
5/ What is the financial impact, lost billings, of waiting on credentials?
This question demonstrates the financial implications of a slow or error-prone credentialing process: Despite the confidence expressed, 43% of respondents said their organization experiences $50,000 or more in lost monthly billings due to credentialing issues.
Another 25%, experience lost billings to the tune of $100,000 every month or more. More than one in 10 reported lost billings in excess of $200,000 per month. Lastly, 10% are unsure of the financial impact.
Q5: What is the estimated financial impact on your organization, in terms of lost billings per month, while waiting for a newly hired provider to complete credentialing? (choose one)
-
- 47% said “less than $50,000” in lost monthly billings;
- 19% said “$50,000-$100,000” in lost monthly billings;
- 13% said “$100,000-$200,000” in lost monthly billings;
- 7% said “$200,000-$300,000” in lost monthly billings;
- 1% said “$300,000-$400,000” in lost monthly billings;
- 1% said “$400,000-$500,000” in lost monthly billings;
- 3% said “more than $500,000” in lost monthly billings; and
- 10% said they were “unsure” about lost monthly billings.
This finding suggests that over the course of a year, around one in four healthcare organizations can trace between $1 and $2 million in lost annual billings to credentialing issues.
(Click for larger image)
6/ What respondents would change about credentialing and onboarding
The final question of the survey was open-ended:
Q6: If you could improve one thing about recruiting, hiring, onboarding or credentialing providers in your organization, what would it be? (open-ended)
More than 200 respondents wrote in answers. In aggregate, these qualitative comments pointed to dissatisfaction with manual efforts in credentialing and onboarding. Some explicitly suggested that technology and standardization could improve the credentialing process.
Below is a sample of some of the verbatim comments:
-
- “The time it takes. 30-60 days is a long time when you are eager to start new things.”
- “More attention needs to [be] made to assure us that things will be handled correctly and efficiently.”
- “Get everything done in 5 business days.”
- “I wish every insurance company would enable you to credential your providers online, so you didn’t have to use any paper form.”
- “Shortening the amount of time it takes, from offer to start date.”
- “I would integrate more AI to reduce human error.”
- “I would make the processes more quickly so we could put employees to work sooner.”
- “Making the credentialing process quicker and easier to get providers started.”
- “The time it takes to onboard and get through credentialing. We lose money when we can’t bill them out.”
- “That we could get providers credentials and other relevant information faster so we can get them onboarded faster.”
About the survey
Intelliworx polled 214 respondents using a commercially available survey panel from December 1, 2025, until December 9, 2025. All respondents work for a U.S.-based healthcare organization in business functions such as human resources (49%), business operations (20%), healthcare recruiting (16%), training & development (7%), finance and accounting (4%) and compliance or credentialing (3%). Respondents also appear to be fairly experienced, with 86% indicating they have five or more years of experience, and nearly half (45%) said they have 10 years of experience in their role.
If you enjoyed this post, you might also like:
Healthcare providers express frustration with payers over denied treatments [survey]